Severing The Connection
Immediate Versus Optimally Delayed Cord Clamping & Why Mothers Should Take Heed
We live in times where birth has been programmed by technocratic institutions, in ways which are a far cry from the physiologic event it was naturally designed to be. There are a number of assaults that are subjected upon mothers and their babies as a result, one of them being immediate clamping of the umbilical cord—the literal lifeline connecting the infant to its only source of blood and nutrition—the placenta.
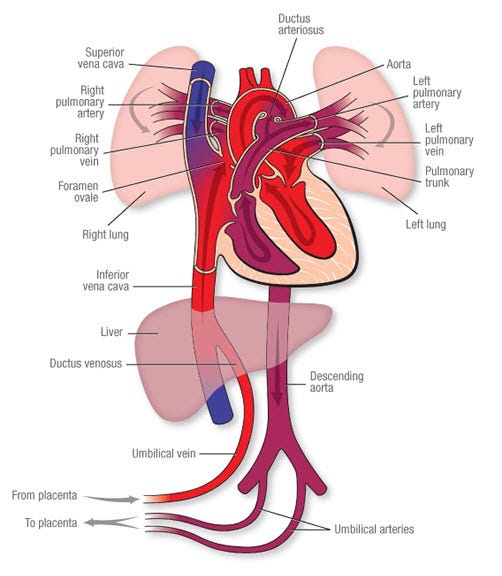
You see, there is a difference in how a fetus “breathes” inside the mother’s womb. It does so by way of not using her lungs, like we do, but rather employs the placenta for these purposes. The placenta, via the umbilical cord vessels, supplies oxygenated blood to the fetus, and carries back waste materials from the fetus back to the mother’s system for removal. As you can imagine, these are blood rich exchanges, which is why, by the time a fetus reaches term, the distribution of blood volume between the fetus, cord and placenta reaches a ratio of approximately 30% of the blood in the cord and placenta while 70% being in the baby, at any given time. Beyond doubt, all of this is baby’s blood.
Optimal placental transfusion is a term that refers to complete exchange of this blood volume from the placenta to the newborn's system. The fetus-to-newborn transition process is designed so that the fetus can transfer most of her placental blood volume into her body at the time of birth, maintaining continuous blood flow to the entire system and facilitating the transition to air breathing. Right when the baby is born, the mother still experiences uterine contractions; these rhythmic surges continue to deliver spurts of blood to the baby, relaxing in between to allow the baby to integrate the blood in her system. This blood volume, that is being transferred gradually from the placenta, helps perfuse all the vital organs, with the GI tract and kidneys needing increased perfusion now that food will be required. Several studies achieved during the past six decades have concluded that adequate placental transfusion dramatically improved perfusion to the newborn's hematologic, urinary, gastrointestinal, neurological, and respiratory systems. If you like to see numbers, an infant who receives a placental transfusion at birth—either from delayed cord clamping or cord milking—acquires more than 30% of blood volume compared to an infant whose cord is immediately severed. It is tragic enough that immediate cord clamping and cutting abruptly halts the placental supply of glucose to the baby’s brain; the newborn’s liver now must begin to work harder on maintaining blood glucose levels by mobilizing its glycogen stores. It’s the liver that basically receives the enriched blood directly from the umbilical vein (which carries oxygenated blood) from the placenta, and hence if liver is not copiously perfused due to this inhumane practice, hypoglycemia may result. Which is a frequent declaration by nurses/neonatologists to quickly jump in and save the hypoglycemic baby from their own failure to give the baby enough time to receive her blood and activate all of her internal organ systems. Deficient perfusion of the liver may also be a factor in poor bilirubin excretion and “physiological” jaundice, which is another commonplace diagnosis in hospital birth.
What’s more, during the third stage of labor while the cord is still pulsating, warm blood from the placenta courses through the newborn. Waiting to ensure that maximum amount of blood volume has transferred to the newborn helps the baby be more resilient to variations in environmental temperature as the baby leaves the consistent temperature of the womb. Such a baby is less likely to suffer from hypothermia because blood is circulating through the placenta (which is still inside a warmer mother) and heating the newborn. After the cord vessels undergo physiologic closure, the newborn has enough blood volume to shift circulation back and forth from her core to the skin to regulate heat loss and retention more effectively than a newborn who is hypovolemic.1
Keep in mind that by allowing and advocating for a delayed cord clamping practice for your baby, you are helping her to receive the residual placental blood (that is rightfully hers) which contains:
• 50% higher amount of iron-rich red blood cells
• A million to 1 billion stem cells
•. Optimum amount of plasma for volume expansion and circulatory support, and
•. Hormones and other substances necessary for her health
Let us translate this information to analyse what this looks like in real life. Ensuring optimal placental transfusion means that your baby will have higher ferritin levels and iron stores by 4-6 months of her age. This means that the odds of anemia of infancy are lower, as well as the negative effects resulting from low iron stores. One study found out that infants with iron deficiency anemia scored lower on the cognitive, motor, social-emotional, and neurophysiologic developmental scale, even if the deficiency was corrected during adulthood.
Similarly, the protective effect of stem cells has been researched extensively, and animal studies have shown the therapeutic properties of the human umbilical cord blood stem cells; these cells selectively repair damaged areas in the body, such as heart and brain, hence proving phenomenal in injury healing process for the receiver's entire life!
Perhaps one of the most profound implications that I learnt—which also became the prime impetus in creating this piece—are the tremendous consequences faced by the baby due to hastening the clamping of the cord. These are twofold:
The abrupt halt in umbilical circulation and hampering of what otherwise should have supposed to be a smooth fetal-to-neonatal transition; the infant experiences a hypovolemic shock (an emergency condition in which severe blood or other fluid loss makes the heart unable to pump enough blood to the body) to their circulatory system, and
A psychological shock, due to overriding the physiologic transition of the baby from the inside of her mother's womb to the outside world, which eventually stays as a memory in our bodies at a cellular level.2
[Take note that during this brief, yet oh-so-critical transition, placental transfusion means that blood is ushered in the extracellular matrix of capillary beds lining the tiny air sacs in the lungs, transforming it from an organ of fluid excretion to an organ of gas exchange].
To drive my point home, let us consider this: in the case of severing a major blood vessel, our body responds by turning on the survival mode created in order to keep us alive. The body is going to direct warmth and blood to the internal organs, like heart, brain and lungs, that are critical for survival and will preferentially constrict capillaries in our extremities, like in our fingers, toes and lips. Being in this state is equated to being in shock as blood and oxygenation to organs and tissues is compromised. And this is exactly what we are doing to our newborns: sending them into a state of shock by tethering their major blood supply immediately and forcing them to switch on their survival mode.
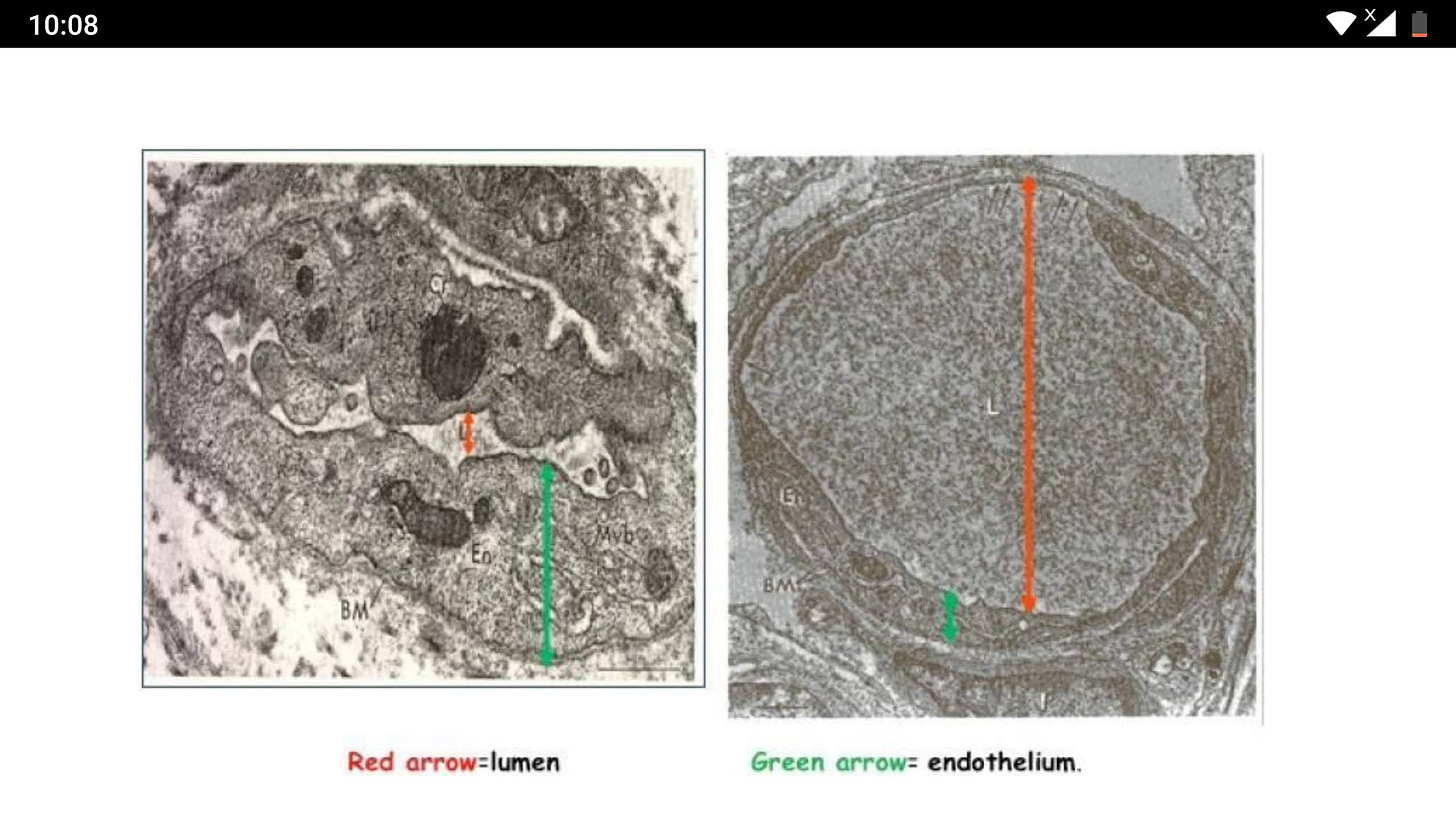
The above image is a visual proof and representation of the shock-theory. These are heel capillaries from infants who received immediate versus delayed cord clamping. Capillary A on the left shows reduced lumen of the capillary indicating blood has been shunted away, while Capillary B on the right shows a wide lumen allowing for maximum exchange of nutrients and waste materials. It is no surprise that Capillary A belongs to infants with immediate cord clamping while Capillary B manifests the physiologic benefits of a gentle and unhastened start to her life that the infant will receive due to delayed cord clamping.
Defending for their baby’s right to receive her own blood therefore falls inside the parents’ domain of control, and something that is worth standing up for, considering the manifold benefits to the baby that result in waiting for the umbilical cord to serve its purpose fully.

A decrease in the volume of circulating blood in the body.